Influencia de la tibolona en la función sexual y seguridad cardiovascular en la mujer posmenopáusica
Influence of tibolone on sexual function and cardiovascular safety in postmenopausal women
Contenido principal del artículo
Resumen
Objetivo: evaluar la influencia de la tibolona en la función sexual, así como la seguridad cardiovascular en la mujer en posmenopausia.
Métodos: se hizo una revisión sistemática de la literatura en diferentes bases de datos electrónicas (CINAHL Plus, Ebsco, Embase, Medline, OVID, Pubmed, REDALYC, Scopus, entre otras), a través de términos de búsqueda libres y estandarizados; entre enero de 1995 y diciembre del 2020. Los desenlaces evaluados incluyeron eficacia de la terapia de reemplazo hormonal con tibolona, su influencia en la función sexual, seguridad cardiovascular e incidencia de efectos adversos.
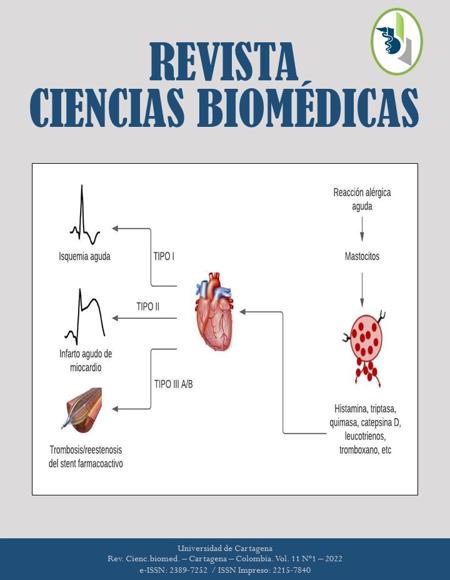
Resultados: se incluyeron 76 estudios. La tibolona es efectiva para el tratamiento de los síntomas vasomotores, sequedad vaginal, alteraciones del ánimo y pérdida de la libido. Reporta efectos beneficiosos en varios aspectos de la función sexual. Su seguridad cardiovascular está avalada al tener actividad vasodilatadora e hipolipemiante con disminución del riesgo coronario durante la posmenopausia temprana, además de poseer propiedades fibrinolíticas (acciones que protegen contra la tromboembolia). Los efectos adversos con mayor incidencia destacan el sangrado vaginal, aumento de peso y sensibilidad mamaria.
Conclusión: La tibolona es tan eficaz como la terapia de reemplazo hormonal convencional para tratar los síntomas vasomotores y prevenir la pérdida ósea, pero superior para el tratamiento de las disfunciones sexuales y elevar el estado de ánimo; con demostrada seguridad cardiovascular y menor incidencia de sangrado vaginal y sensibilidad / dolor mamario. Es necesario el diseño de ensayos clínicos controlados aleatorizados, para demostrar los hallazgos de la presente revisión.
Palabras clave
Descargas
Datos de publicación
Perfil evaluadores/as N/D
Declaraciones de autoría
- Sociedad académica
- Universidad de Cartagena
- Editorial
- Universidad de Cartagena
Detalles del artículo
Referencias (VER)
Oldenhave A, Jaszmann LJ, Haspels AA, Everaerd WT. Impact of climacteric on well-being. A survey based on 5213 women 39 to 60 years old. Am J Obstet Gynecol. 1993; 168(3 Pt 1):772-80. http://dx.doi.org/10.1016/s0002-9378(12)90817-0 DOI: https://doi.org/10.1016/S0002-9378(12)90817-0
Jenabi E, Shobeiri F, Hazavehei SM, Roshanaei G. Assessment of Questionnaire Measuring Quality of Life in Menopausal Women: A Systematic Review. Oman Med J. 2015; 30(3):151-6. http://dx.doi.org/10.5001/omj.2015.34 DOI: https://doi.org/10.5001/omj.2015.34
Li C, Samsioe G, Borgfeldt C, Lidfeldt J, Agardh CD, Nerbrand C. Menopause-related symptoms: what are the background factors? A prospective population-based cohort study of Swedish women (The Women's Health in Lund Area study). Am J Obstet Gynecol. 2003; 189(6):1646-53. http://dx.doi.org/10.1016/s0002-9378(03)00872-x DOI: https://doi.org/10.1016/S0002-9378(03)00872-X
Thurston RC, Joffe H. Vasomotor symptoms and menopause: findings from the Study of Women's Health across the Nation. Obstet Gynecol Clin North Am. 2011; 38(3):489-501. http://dx.doi.org/10.1016/j.ogc.2011.05.006 DOI: https://doi.org/10.1016/j.ogc.2011.05.006
Espitia De la Hoz FJ. Prevalence of genitourinary syndrome of menopause and impact on sexuality of women in Quindío (Colombia), 2013-2016. Rev Colomb Obstet Ginecol. 2018; 69(4):249-59. https://doi.org/10.18597/rcog.3111 DOI: https://doi.org/10.18597/rcog.3111
Warren MP, Halpert S. Hormone replacement therapy: controversies, pros and cons. Best Pract Res Clin Endocrinol Metab. 2004; 18(3):317-32. https://doi.org/10.1016/j.beem.2004.02.005 DOI: https://doi.org/10.1016/j.beem.2004.02.005
Björn I, Bäckström T, Lalos A, Sundström-Poromaa I. Adverse mood effects during postmenopausal hormone treatment in relation to personality traits. Climacteric. 2006; 9(4):290-7. https://doi.org/10.1080/13697130600865766 DOI: https://doi.org/10.1080/13697130600865766
Utian WH, Shoupe D, Bachmann G, Pinkerton JV, Pickar JH. Relief of vasomotor symptoms and vaginal atrophy with lower doses of conjugated equine estrogens and medroxyprogesterone acetate. Fertil Steril. 2001; 75(6):1065-79. https://doi.org/10.1016/s0015-0282(01)01791-5 DOI: https://doi.org/10.1016/S0015-0282(01)01791-5
Johansen N, Liavaag AH, Tanbo TG, Dahl AA, Pripp AH, Michelsen TM. Sexual activity and functioning after risk-reducing salpingo-oophorectomy: Impact of hormone replacement therapy. Gynecol Oncol. 2016; 140(1):101-6. https://doi.org/10.1016/j.ygyno.2015.11.016 DOI: https://doi.org/10.1016/j.ygyno.2015.11.016
Hodis HN, Mack WJ. Hormone replacement therapy and the association with coronary heart disease and overall mortality: clinical application of the timing hypothesis. J Steroid Biochem Mol Biol. 2014; 142:68-75. https://doi.org/10.1016/j.jsbmb.2013.06.011 DOI: https://doi.org/10.1016/j.jsbmb.2013.06.011
The NAMS 2017 Hormone Therapy Position Statement Advisory Panel. The 2017 hormone therapy position statement of The North American Menopause Society. Menopause. 2017; 24(7):728-53. https://doi.org/10.1097/GME.0000000000000921 DOI: https://doi.org/10.1097/GME.0000000000000921
Preston RA. Comparative effects of conventional vs. novel hormone replacement therapy on blood pressure in postmenopausal women. Climacteric. 2009; 12 Suppl 1:66-70. https://doi.org/10.1080/13697130902775788 DOI: https://doi.org/10.1080/13697130902775788
Kenemans P. Tibolone: how does its mechanism of action translate into clinical effects. Maturitas. 2004; 48 Suppl 1:S1-3. https://doi.org/10.1016/j.maturitas.2004.02.014 DOI: https://doi.org/10.1016/j.maturitas.2004.02.014
Wang PH, Horng HC, Cheng MH, Chao HT, Chao KC. Standard and low-dose hormone therapy for postmenopausal women--focus on the breast. Taiwan J Obstet Gynecol. 2007; 46(2):127-34. https://doi.org/10.1016/S1028-4559(07)60006-0 DOI: https://doi.org/10.1016/S1028-4559(07)60006-0
Modelska K, Cummings S. Tibolone for postmenopausal women: systematic review of randomized trials. J Clin Endocrinol Metab. 2002; 87(1):16-23. https://doi.org/10.1210/jcem.87.1.8141 DOI: https://doi.org/10.1210/jcem.87.1.8141
Timmer CJ, Verheul HA, Doorstam DP. Pharmacokinetics of tibolone in early and late postmenopausal women. Br J Clin Pharmacol. 2002; 54(2):101-6. https://doi.org/10.1046/j.1365-2125.2002.01619.x DOI: https://doi.org/10.1046/j.1365-2125.2002.01619.x
Crona N, Samsioe G, Lindberg UB, Silfverstolpe G. Treatment of climacteric complaints with Org OD 14: a comparative study with oestradiol valerate and placebo. Maturitas. 1988; 9(4):303-8. https://doi.org/10.1016/0378-5122(88)90095-3 DOI: https://doi.org/10.1016/0378-5122(88)90095-3
Kicovic PM, Cortés-Prieto J, Luisi M, Milojevic S, Franchi F. Placebo-controlled cross-over study of effects of Org OD 14 in menopausal women. Reproduccion. 1982; 6(2):81-91.
Punnonen R, Liukko P, Cortes-Prieto J, Eydam F, Milojevic S, Trévoux R, et al. Multicentre study of effects of Org OD 14 on endometrium, vaginal cytology and cervical mucus in post-menopausal and oophorectomized women. Maturitas. 1984; 5(4):281-6. https://doi.org/10.1016/0378-5122(84)90023-9 DOI: https://doi.org/10.1016/0378-5122(84)90023-9
de Gooyer ME, Deckers GH, Schoonen WG, Verheul HA, Kloosterboer HJ. Receptor profiling and endocrine interactions of tibolone. Steroids. 2003; 68(1):21-30. https://doi.org/10.1016/s0039-128x(02)00112-5 DOI: https://doi.org/10.1016/S0039-128X(02)00112-5
Jelinek J, Kappen A, Schönbaum E, Lomax P. A primate model of human postmenopausal hot flushes. J Clin Endocrinol Metab. 1984; 59(6):1224-8. https://doi.org/10.1210/jcem-59-6-1224 DOI: https://doi.org/10.1210/jcem-59-6-1224
Landgren MB, Helmond FA, Engelen S. Tibolone relieves climacteric symptoms in highly symptomatic women with at least seven hot flushes and sweats per day. Maturitas. 2005; 50(3):222-30. https://doi.org/10.1016/j.maturitas.2004.06.001 DOI: https://doi.org/10.1016/j.maturitas.2004.06.001
Espitia De La Hoz FJ. Terapia de reemplazo hormonal combinada con testosterona para el tratamiento del trastorno del deseo sexual hipoactivo en mujeres en climaterio. Arch Med (Manizales) 2020; 20(1):71-85. https://doi.org/10.30554/archmed.20.1.3388.2020 DOI: https://doi.org/10.30554/archmed.20.1.3388.2020
Verheul HA, Blok LJ, Burger CW, Hanifi-Moghaddam P, Kloosterboer HJ. Levels of tibolone and estradiol and their nonsulfated and sulfated metabolites in serum, myometrium, and vagina of postmenopausal women following treatment for 21 days with tibolone, estradiol, or estradiol plus medroxyprogestrone acetate. Reprod Sci. 2007; 14(2):160-8. https://doi.org/10.1177/1933719106298684 DOI: https://doi.org/10.1177/1933719106298684
Albertazzi P, Di Micco R, Zanardi E. Tibolone: a review. Maturitas. 1998; 30(3):295-305. https://doi.org/10.1016/s0378-5122(98)00059-0 DOI: https://doi.org/10.1016/S0378-5122(98)00059-0
Formoso G, Perrone E, Maltoni S, Balduzzi S, D'Amico R, Bassi C, et al. Short and long term effects of tibolone in postmenopausal women. Cochrane Database Syst Rev. 2012; (2):CD008536. https://doi.org/10.1002/14651858.CD008536.pub2 DOI: https://doi.org/10.1002/14651858.CD008536.pub2
Moore RA. Livial: a review of clinical studies. Br J Obstet Gynaecol. 1999; 106 Suppl 19:1-21.
Ziaei S, Moghasemi M, Faghihzadeh S. Comparative effects of conventional hormone replacement therapy and tibolone on climacteric symptoms and sexual dysfunction in postmenopausal women. Climacteric. 2010; 13(2):147-56. https://doi.org/10.1080/13697130903009195 DOI: https://doi.org/10.3109/13697130903009195
Vos RM, Krebbers SF, Verhoeven CH, Delbressine LP. The in vivo human metabolism of tibolone. Drug Metab Dispos. 2002; 30(2):106-12. https://doi.org/10.1124/dmd.30.2.106 DOI: https://doi.org/10.1124/dmd.30.2.106
Palacios S, Menendez C, Jurado AR, Castaño R, Vargas JC. Changes in sex behaviour after menopause: effects of tibolone. Maturitas. 1995; 22(2):155-61. https://doi.org/10.1016/0378-5122(95)00930-j DOI: https://doi.org/10.1016/0378-5122(95)00930-J
Kökçü A, Cetinkaya MB, Yanik F, Alper T, Malatyalioğlu E. The comparison of effects of tibolone and conjugated estrogen-medroxyprogesterone acetate therapy on sexual performance in postmenopausal women. Maturitas. 2000; 36(1):75-80. https://doi.org/10.1016/s0378-5122(00)00134-1 DOI: https://doi.org/10.1016/S0378-5122(00)00134-1
Omu F, Elbiaa A, Ghafour A, Gadalla I, Omu A. Beneficial Effects of Tibolone on Sexual Dys-function in Women with Premature Ovarian Failure (POF). Health. 2016; 8(9):857-67. https://doi.org/10.4236/health.2016.89090 DOI: https://doi.org/10.4236/health.2016.89090
Dören M, Rübig A, Coelingh Bennink HJ, Holzgreve W. Differential effects on the androgen status of postmenopausal women treated with tibolone and continuous combined estradiol and norethindrone acetate replacement therapy. Fertil Steril. 2001; 75(3):554-9. https://doi.org/10.1016/s0015-0282(00)01768-4 DOI: https://doi.org/10.1016/S0015-0282(00)01768-4
van der Stege JG, Groen H, van Zadelhoff SJ, Lambalk CB, Braat DD, van Kasteren YM, et al. Decreased androgen concentrations and diminished general and sexual well-being in women with premature ovarian failure. Menopause. 2008; 15(1):23-31. https://doi.org/10.1097/gme.0b013e3180f6108c DOI: https://doi.org/10.1097/gme.0b013e3180f6108c
Drillich A, Davis SR. Androgen therapy in women: what we think we know. Exp Gerontol. 2007; 42(6):457-62. https://doi.org/10.1016/j.exger.2007.02.005 DOI: https://doi.org/10.1016/j.exger.2007.02.005
Kloosterboer HJ. Tibolone: a steroid with a tissue-specific mode of action. J Steroid Biochem Mol Biol. 2001; 76(1-5):231-8. https://doi.org/10.1016/s0960-0760(01)00044-9 DOI: https://doi.org/10.1016/S0960-0760(01)00044-9
Laan E, van Lunsen RH, Everaerd W. The effects of tibolone on vaginal blood flow, sexual desire and arousability in postmenopausal women. Climacteric. 2001; 4(1):28-41. DOI: https://doi.org/10.1080/cmt.4.1.28.41
Wu MH, Pan HA, Wang ST, Hsu CC, Chang FM, Huang KE. Quality of life and sexuality changes in postmenopausal women receiving tibolone therapy. Climacteric. 2001; 4(4):314-9. DOI: https://doi.org/10.1080/cmt.4.4.314.319
Valdivia I, Campodónico I, Tapia A, Capetillo M, Espinoza A, Lavín P. Effects of tibolone and continuous combined hormone therapy on mammographic breast density and breast histochemical markers in postmenopausal women. Fertil Steril. 2004; 81(3):617-23. https://doi.org/10.1016/j.fertnstert.2003.07.041 DOI: https://doi.org/10.1016/j.fertnstert.2003.07.041
Wender MC, Edelweiss MI, Campos LS, de Castro JA, Spritzer PM. Endometrial assessment in women using tibolone or placebo: 1-year randomized trial and 2-year observational study. Menopause. 2004; 11(4):423-9. https://doi.org/10.1097/01.gme.0000109315.11228.ac DOI: https://doi.org/10.1097/01.GME.0000109315.11228.AC
Kenemans P, Speroff L; International Tibolone Consensus Group. Tibolone: clinical recommendations and practical guidelines. A report of the International Tibolone Consensus Group. Maturitas. 2005; 51(1):21-8. https://doi.org/10.1016/j.maturitas.2005.02.011 DOI: https://doi.org/10.1016/j.maturitas.2005.02.011
Roux C, Pelissier C, Fechtenbaum J, Loiseau-Peres S, Benhamou CL. Randomized, double-masked, 2-year comparison of tibolone with 17beta-estradiol and norethindrone acetate in preventing postmenopausal bone loss. Osteoporos Int. 2002; 13(3):241-8. https://doi.org/10.1007/s001980200021 DOI: https://doi.org/10.1007/s001980200021
Lippuner K, Haenggi W, Birkhaeuser MH, Casez JP, Jaeger P. Prevention of postmenopausal bone loss using tibolone or conventional peroral or transdermal hormone replacement therapy with 17beta-estradiol and dydrogesterone. J Bone Miner Res. 1997; 12(5):806-12. https://doi.org/10.1359/jbmr.1997.12.5.806 DOI: https://doi.org/10.1359/jbmr.1997.12.5.806
Rymer J, Robinson J, Fogelman I. Ten years of treatment with tibolone 2.5 mg daily: effects on bone loss in postmenopausal women. Climacteric. 2002; 5(4):390-8. DOI: https://doi.org/10.1080/cmt.5.4.390.398
Morris EP, Denton ER, Robinson J, MacDonald LM, Rymer JM. High resolution ultrasound assessment of the carotid artery: its relevance in postmenopausal women and the effects of tibolone on carotid artery ultrastructure. Climacteric. 1999; 2(1):13-20. https://doi.org/10.3109/13697139909025558 DOI: https://doi.org/10.3109/13697139909025558
Cagnacci A, Baldassari F, Arangino S, Alessandrini C, Volpe A. Administration of tibolone decreases 24 h heart rate but not blood pressure of post-menopausal women. Maturitas. 2004; 48(2):155-60. https://doi.org/10.1016/j.maturitas.2003.08.011 DOI: https://doi.org/10.1016/j.maturitas.2003.08.011
Ostberg JE, Damjanovic T, Dimkovic N, Byrne D, Mikhailidis DP, Prelevic GM. Effect of tibolone on markers of cardiovascular disease risk in postmenopausal women undergoing hemodialysis: a pilot study. Fertil Steril. 2004; 81(6):1624-31. https://doi.org/10.1016/j.fertnstert.2003.11.033 DOI: https://doi.org/10.1016/j.fertnstert.2003.11.033
Christodoulakos GE, Lambrinoudaki IV, Panoulis CP, Papadias CA, Kouskouni EE, Creatsas GC. Effect of hormone replacement therapy, tibolone and raloxifene on serum lipids, apolipoprotein A1, apolipoprotein B and lipoprotein(a) in Greek postmenopausal women. Gynecol Endocrinol. 2004; 18(5):244-57. https://doi.org/10.1080/09513590410001715207 DOI: https://doi.org/10.1080/09513590410001715207
Vassalle C, Cicinelli E, Lello S, Mercuri A, Battaglia D, Maffei S. Effects of menopause and tibolone on different cardiovascular biomarkers in healthy women. Gynecol Endocrinol. 2011; 27(3):163-9. https://doi.org/10.3109/09513590.2010.488770. DOI: https://doi.org/10.3109/09513590.2010.488770
von Eckardstein A, Schmiddem K, Hövels A, Gülbahçe E, Schuler-Lüttmann S, Elbers J, et al. Lowering of HDL cholesterol in post-menopausal women by tibolone is not associated with changes in cholesterol efflux capacity or paraoxonase activity. Atherosclerosis. 2001; 159(2):433-9. https://doi.org/10.1016/s0021-9150(01)00522-6 DOI: https://doi.org/10.1016/S0021-9150(01)00522-6
Simoncini T, Mannella P, Fornari L, Caruso A, Varone G, Garibaldi S, et al. Tibolone activates nitric oxide synthesis in human endothelial cells. J Clin Endocrinol Metab. 2004; 89(9):4594-600. https://doi.org/10.1210/jc.2003-032189. DOI: https://doi.org/10.1210/jc.2003-032189
Cicinelli E, Ignarro LJ, Galantino P, Pinto V, Barba B, Schonauer S. Effects of tibolone on plasma levels of nitric oxide in postmenopausal women. Fertil Steril. 2002; 78(3):464-8. https://doi.org/10.1016/s0015-0282(02)03295-8 DOI: https://doi.org/10.1016/S0015-0282(02)03295-8
Simoncini T, Genazzani AR. Tibolone inhibits leukocyte adhesion molecule expression in human endothelial cells. Mol Cell Endocrinol. 2000; 162(1-2):87-94. https://doi.org/10.1016/s0303-7207(00)00206-9 DOI: https://doi.org/10.1016/S0303-7207(00)00206-9
Aguayo-Cerón KA, Morales-González JA, Gutiérrez-Iglesias G, Parra-Barrera A, Jiménez-Zamarripa CA, Ocharán-Hernández ME, et al. Efecto Regulador de Tibolona sobre la Actividad Antiinflamatoria del Macrófago. Revista Mexicana De Ingeniería Biomédica. 2019; 40(3):1-10. https://doi.org/10.17488/RMIB.40.3.1 DOI: https://doi.org/10.17488/RMIB.40.3.1
North American Menopause Society. The 2012 hormone therapy position statement of: The North American Menopause Society. Menopause. 2012; 19(3):257-71. https://doi.org/10.1097/gme.0b013e31824b970a DOI: https://doi.org/10.1097/gme.0b013e31824b970a
Stuenkel CA, Davis SR, Gompel A, Lumsden MA, Murad MH, Pinkerton JV, et al. Treatment of Symptoms of the Menopause: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2015; 100(11):3975-4011. https://doi.org/10.1210/jc.2015-2236 DOI: https://doi.org/10.1210/jc.2015-2236
Eilertsen AL, Qvigstad E, Andersen TO, Sandvik L, Sandset PM. Conventional-dose hormone therapy (HT) and tibolone, but not low-dose HT and raloxifene, increase markers of activated coagulation. Maturitas. 2006; 55(3):278-87. https://doi.org/10.1016/j.maturitas.2006.04.012 DOI: https://doi.org/10.1016/j.maturitas.2006.04.012
Appt SE, Törmälä R, Franke AA, Mikkola TS, Tikkanen MJ, Ylikorkala O, et al. Soy-tibolone combination - effect on lipids in postmenopausal monkeys and women. Maturitas. 2008; 60(3-4):216-22. https://doi.org/10.1016/j.maturitas.2008.06.003 DOI: https://doi.org/10.1016/j.maturitas.2008.06.003
Bjarnason NH, Bjarnason K, Haarbo J, Bennink HJ, Christiansen C. Tibolone: influence on markers of cardiovascular disease. J Clin Endocrinol Metab. 1997; 82(6):1752-6. https://doi.org/10.1210/jcem.82.6.3995 DOI: https://doi.org/10.1210/jcem.82.6.3995
Register TC, Wagner JD, Zhang L, Hall J, Clarkson TB. Effects of tibolone and conventional hormone replacement therapies on arterial and hepatic cholesterol accumulation and on circulating endothelin-1, vascular cell adhesion molecule-1, and E-selectin in surgically menopausal monkeys. Menopause. 2002; 9(6):411-21. https://doi.org/10.1097/00042192-200211000-00006 DOI: https://doi.org/10.1097/00042192-200211000-00006
Stark J, Varbiro S, Sipos M, Tulassay Z, Sara L, Adler I, et al. Antioxidant effect of the active metabolites of tibolone. Gynecol Endocrinol. 2015; 31(1):31-5. https://doi.org/10.3109/09513590.2014.943727 DOI: https://doi.org/10.3109/09513590.2014.943727
Dubey RK, Gillespie DG, Grögli M, Kloosterboer HJ, Imthurn B. Tibolone and its metabolites induce antimitogenesis in human coronary artery smooth muscle cells: role of estrogen, progesterone, and androgen receptors. J Clin Endocrinol Metab. 2004; 89(2):852-9. https://doi.org/10.1210/jc.2003-031272 DOI: https://doi.org/10.1210/jc.2003-031272
Castelo-Branco C, Casals E, Figueras F, Sanjuan A, Vicente JJ, Balasch J, et al. Two-year prospective and comparative study on the effects of tibolone on lipid pattern, behavior of apolipoproteins AI and B. Menopause. 1999 Summer; 6(2):92-7. DOI: https://doi.org/10.1097/00042192-199906020-00004
Nathorst-Böös J, Hammar M. Effect on sexual life--a comparison between tibolone and a continuous estradiol-norethisterone acetate regimen. Maturitas. 1997; 26(1):15-20. https://doi.org/10.1016/s0378-5122(96)01069-9 DOI: https://doi.org/10.1016/S0378-5122(96)01069-9
Espitia De La Hoz FJ, Marega O, Orozco Gallego H. Manejo farmacológico de la disfunción sexual femenina en la postmenopausia, con tibolona y testosterona. Revista de Sexología. 2016; 5(2):9-18.
Nijland EA, Weijmar Schultz WC, Nathorst-Boös J, Helmond FA, Van Lunsen RH, Palacios S, et al. Tibolone and transdermal E2/NETA for the treatment of female sexual dysfunction in naturally menopausal women: results of a randomized active-controlled trial. J Sex Med. 2008; 5(3):646-56. https://doi.org/10.1111/j.1743-6109.2007.00726.x DOI: https://doi.org/10.1111/j.1743-6109.2007.00726.x
Baños G, Guarner V, Pérez-Torres I. Sex steroid hormones, cardiovascular diseases and the metabolic syndrome. Cardiovasc Hematol Agents Med Chem. 2011; 9(3):137-46. https://doi.org/10.2174/187152511797037547 DOI: https://doi.org/10.2174/187152511797037547
Kotani K, Sahebkar A, Serban C, Andrica F, Toth PP, Jones SR, et al. Tibolone decreases Lipoprotein(a) levels in postmenopausal women: A systematic review and meta-analysis of 12 studies with 1009 patients. Atherosclerosis. 2015; 242(1):87-96. https://doi.org/10.1016/j.atherosclerosis.2015.06.056 DOI: https://doi.org/10.1016/j.atherosclerosis.2015.06.056
Parkin DE, Smith D, Al Azzawi F, Lindsay R, Hart DM. Effects of long-term Org OD 14 administration on blood coagulation in climacteric women. Maturitas. 1987; 9(1):95-101. https://doi.org/10.1016/0378-5122(87)90057-0 DOI: https://doi.org/10.1016/0378-5122(87)90057-0
Tax L, Kicovic PM. Clinical profile of Org OD14. Maturitas 1984; 6:196. DOI: https://doi.org/10.1016/0378-5122(84)90212-3
Yates RW, Richards A, McEwan HP, Coutts JR, Walker ID, Davidson JF. Hormonal and fibrinolytic effects of the synthetic steroid Org OD14 in menopausal women. Maturitas 1984; 6:210. DOI: https://doi.org/10.1016/0378-5122(84)90228-7
Archer DF, Hendrix S, Gallagher JC, Rymer J, Skouby S, Ferenczy A, et al. Endometrial effects of tibolone. J Clin Endocrinol Metab. 2007; 92(3):911-8. https://doi.org/10.1210/jc.2006-2207. DOI: https://doi.org/10.1210/jc.2006-2207
Bundred NJ, Kenemans P, Yip CH, Beckmann MW, Foidart JM, Sismondi P, et al. Tibolone increases bone mineral density but also relapse in breast cancer survivors: LIBERATE trial bone substudy. Breast Cancer Res. 2012; 14(1):R13. https://doi.org/10.1186/bcr3097. DOI: https://doi.org/10.1186/bcr3097
Bringer J, Raingeard I, Lefebre P, Renard E. Ménopause. Vers un traitement «a la carte». Ann Endocrinol. 2003; 64:337-44.
McKinney KA, Thompson W. A practical guide to prescribing hormone replacement therapy. Drugs. 1998; 56:49-57. DOI: https://doi.org/10.2165/00003495-199856010-00005
Modelska K, Cummings S. Female sexual dysfunction in postmenopausal women: systematic review of placebo-controlled trials. Am J Obstet Gynecol. 2003; 188(1):286-93. https://doi.org/10.1067/mob.2003.117 DOI: https://doi.org/10.1067/mob.2003.117


 PDF
PDF
 FLIP
FLIP





