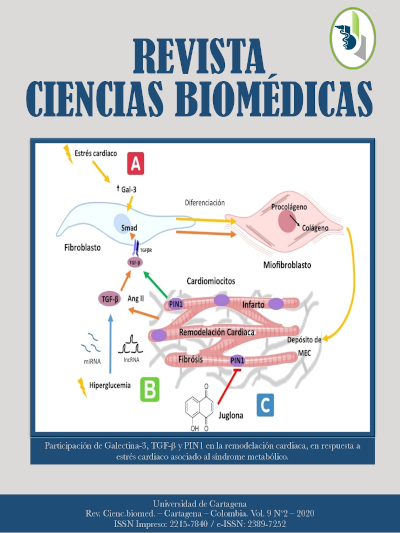
Cambios moleculares en la remodelación cardiaca por síndrome metabólico.
Molecular changes in cardiac remodeling due to metabolic syndrome.
Contenido principal del artículo
Resumen
Introducción: el síndrome metabólico (SM) es un conjunto de anormalidades caracterizadas por el aumento de presión arterial, elevación de la glucemia en ayuno, dislipidemias, obesidad y/o diabetes, en donde se encuentran implicadas diversas moléculas que participan en la comunicación intracelular. Objetivo: se describe la función y mecanismo de señalización intracelular que involucra a algunas de las moléculas que llevan a cabo procesos de remodelación cardiaca y son de especial interés como biomarcadores. Métodos: se realizó una selección de literatura que nos describiera la participación de las moléculas en el proceso de remodelación cardiaca como resultado del SM. Conclusiones: el SM y la falla cardiaca se encuentra íntimamente vinculados por la modulación de diversas vías de señalización intracelular que contribuyen a la remodelación cardiaca, generando cambios estructurales modificando la fisiopatología del cardiomiocito.
Palabras clave:
Descargas
Detalles del artículo
Referencias (VER)
Al-Daghri NM, Alkharfy KM, Al-Saleh Y, Al-Attas OS, Alokail MS, Al-Othman A, et al. Modest reversal of metabolic syndrome manifestations with vitamin D status correction: A 12-month prospective study. Metabolism [Internet]. 2012; 61(5): 661-6. https://doi.org/10.1016/j.metabol.2011.09.017
Tadic M, Cuspidi C. Childhood obesity and cardiac remodeling: From cardiac structure to myocardial mechanics. J Cardiovasc Med. 2015;16(8):538-46. https://doi.org/10.2459/JCM.0000000000000261
XuZ,SunJ,TongQ,LinQ,QianL,ParkY,etal.The role of ERK1/2 in the development of diabetic cardiomyopathy. Int J Mol Sci. 2016;17(12):1-17. https://doi.org/10.3390/ijms17122001
Martínez-Martínez E, López-Ándres N, Jurado-López R, Rousseau E, Bartolomé MV, Fernández-Celis A, et al. Galectin-3 participates in cardiovascular remodeling associated with obesity. Hypertension. 2015;66(5):961- 9. https://doi.org/10.1161/HYPERTENSIONAHA.115.06032
De Boer RA, V an Der V elde AR. Galectin-3: A new biomarker for heart failure progression and prognosis. Laboratoriums Medizin. 2013;37(5):251-60. https://doi.org/10.1515/labmed-2012-0073
Bobronnikova L. Galectin-3 as a potential biomarker of metabolic disorders and cardiovascular remodeling in patients with hypertension and type 2 diabetes. Vessel Plus. 2017;1(2):61-7. https://doi.org/10.20517/2574-1209.2016.10
Yue Y, Meng K, Pu Y, Zhang X. Transforming growth factor beta (TGF-β) mediates cardiac fibrosis and induces diabetic cardiomyopathy. Diabetes Res Clin Pract [Internet]. 2017; 133: 124-30. Available from: https://doi.org/10.1016/j.diabres.2017.08.018
Liu G, Ma C, Yang H, Zhang PY. Transforming growth factor β and its role in heart disease. Exp Ther Med. 2017;13(5):2123-8. https://doi.org/10.3892/etm.2017.4246
Liu X, Liang E, Song X, Du Z, Zhang Y, Zhao Y. Inhibition of Pin1 alleviates myocardial fibrosis and dysfunction in STZ-induced diabetic mice. Biochem Biophys Res Commun 2016; 479(1): 109-15. https://doi.org/10.1016/j.bbrc.2016.09.050
Shaker YM, Soliman HA, Ezzat E, Hussein NS, Ashour E, Donia A, et al. Serum and urinary transforming growth factor beta 1 as biochemical markers in diabetic nephropathy patients. Beni-Suef Univ J Basic Appl Sci. 2014;3(1):16-23. https://doi.org/10.1016/j.bjbas.2014.02.002
Huang GL, Qiu JH, Li BBin, Wu JJ, Lu Y, Liu XY, et al. Prolyl isomerase pin1 regulated signaling pathway revealed by pin1 +/+ and Pin1 -/- mouse embryonic fibroblast cells. Pathol Oncol Res. 2013; 19(4): 667-75. https://doi.org/10.1007/s12253-013-9629-x
Turner, Blythe. Cardiac Fibroblast p38 MAPK: A Critical Regulator of Myocardial Remodeling. J Cardiovasc Dev Dis. 2019;6(3):27. https://doi.org/10.3390/jcdd6030027
Muslin JA. MAPK Signaling in cardiovascular health and desease: Molecular mechanism and therapeutic targets. Clin Sci. 2009;115(7):203-18. https://doi.org/10.1042/CS20070430
Wang S, Ding L, Ji H, Xu Z, Liu Q, Zheng Y. Therole of p38 MAPK in the development of diabetic cardiomyopathy. Int J Mol Sci. 2016;17(7):1-14. https://doi.org/10.3390/ijms18010001
Craige SM, Chen K, Blanton RM, Keaney JF, Kant S. JNK and cardiometabolic dysfunction. Biosci Rep. 2019;39(7):1-18. https://doi.org/10.1042/BSR20190267
Pal M, Febbraio MA, Lancaster GI. The roles of c-Jun NH2-terminal kinases (JNKs) in obesity and insulin resistance. J Physiol. 2016; 594(2): 267-79. https://doi.org/10.1113/JP271457
Schumacher-Bass SM, Traynham CJ, Koch WJ. G protein-coupled receptor kinase 2 as a therapeutic target for heart failure. Drug Discov Today Ther Strateg. 2012;9(4):1-14. https://doi.org/10.1016/j.ddstr.2014.01.002
Woodall MC, Ciccarelli M, Woodall BP, Koch WJ. GRK2 - A Link Between Myocardial Contractile Function and Cardiac Metabolism. Circ Res. 2014;114(10):1661-70. https://doi.org/10.1161/CIRCRESAHA.114.300513
Goncąlves N, Falcaõ-Pires I, Leite-Moreira AF. Adipokines and their receptors: Potential new targets in cardiovascular diseases. Future Med Chem. 2015;7(2):139-57. https://doi.org/10.4155/fmc.14.147
Hui X, Lam KS, Vanhoutte PM, Xu A. Adiponectin and cardiovascular health: An update. Br J Pharmacol. 2012;165(3):574-90. https://doi.org/10.1111/j.1476-5381.2011.01395.x
Imo A. E, David C. GJ, Carlos J. R, Haiying C, Alain G. B. Mechanisms of heart failure in obesity. Obes Res Clin Pr. 2014;8(6):e540-8. https://doi.org/10.1016/j.orcp.2013.12.005
Katsiki N, Mikhailidis DP , Banach M. Leptin, cardiovascular diseases and type 2 diabetes mellitus review-article. Acta Pharmacol Sin. 2018;39(7):1176-88. https://doi.org/10.1038/aps.2018.40
Fujioka S, Niu J, Schmidt C, Sclabas GM, Peng B, Uwagawa T, et al. NF-kβ and AP-1 Connection : Mechanism of NF-kβ Dependent Regulation of AP-1 Activity. 2004; 24(17): 7806-19. https://doi.org/10.1128/MCB.24.17.7806-7819.2004
Craig R, Wagner M, McCardle T, Craig AG, Glembotski CC. The Cytoprotective Effects of the Glycoprotein 130 Receptor-coupled Cytokine, Cardiotrophin-1, Require Activation of NF-κB. J Biol Chem. 2001;276(40):37621- 9. https://doi.org/10.1074/jbc.M103276200
Hernández-Gutiérrez S, Rojas-del Castillo E. edigraphic.com. El Pap del factor transcripción NF-κB en la célula cardíaca. 2005;75:363-70.
Higuchi M, Manna SK, Sasaki R, Aggarwal BB. Regulation of the activation of nuclear factor κB by mitochondrial respiratory function: Evidence for the reactive oxygen species-dependent and -independent pathways. Antioxidants Redox Signal. 2002; 4(6): 945-55. https://doi.org/10.1089/152308602762197489
Purcell NH, Tang G, Yu C, Mercurio F, DiDonato JA, Lin A. Activation of NF-κB is required for hypertrophic growth of primary rat neonatal ventricular cardiomyocytes. Proc Natl Acad Sci U S A. 2001;98(12):6668-73. https://doi.org/10.1073/pnas.111155798
Park KR, Kwon MS, An JY, Lee JG, Youn HS, Lee Y, et al. Structural implications of Ca2+-dependent actin- bundling function of human EFhd2/Swiprosin-1. Sci Rep. 2016;6(July):1-15. https://doi.org/10.1038/srep39095
Huh YH, Kim SH, Chung KH, Oh S, Kwon MS, Choi HW, et al. Swiprosin-1 modulates actin dynamics by regulating the F-actin accessibility to cofilin. Cell Mol Life Sci. 2013; 70(24): 4841-54. https://doi.org/10.1007/s00018-013-1447-5
Schreckenberg R, Pöling J, Lörchner H. Swiprosin- 1/EFhD-2 Expression in Cardiac Remodeling and Post- Infarct Repair : Effect of Ischemic Conditioning. 2020; 2: 1-13.
Nippert F, Schreckenberg R, Hess A, Weber M, Schlüter KD. The effects of swiprosin-1 on the formation of pseudopodia-like structures and β- adrenoceptor coupling in cultured adult rat ventricular cardiomyocytes. PLoS One. 2016; 11(12): 1-15. https://doi.org/10.1371/journal.pone.0167655


 PDF
PDF
 FLIP
FLIP